Occupational Hygiene - Ototoxic Chemicals
On this page
- What is the auditory system and what is its function?
- What are the parts of our auditory system?
- What is ototoxicity, and what are ototoxicants?
- How do ototoxicants damage the auditory system?
- What are possible health effects from ototoxicants and what are the symptoms?
- What chemicals cause ototoxicity?
- What is OTO notation and what is its purpose?
- What workplaces use ototoxic chemical substances and which occupations may be exposed?
- How does a workplace know if a hazardous product causes ototoxicity?
- What are the employer’s responsibilities for protecting workers from ototoxicants?
- What are the worker’s responsibilities when working with ototoxicants?
What is the auditory system and what is its function?
Back to topThe auditory system is responsible for our sense of hearing. It includes the outer, middle, and inner ears, as well as the central auditory nervous system. The auditory system is able to change a wide range of mechanical signals into a complex series of electrical signals. The brain then interprets these signals into a sound that we recognize and understand.
What are the parts of our auditory system?
Back to topThe auditory system consists of many different parts and sections. See the figure below for an image of the auditory system. Successful hearing requires all of these parts and sections to function properly.
- Outer ear: The pinna sits on the side of your ear and collects the sounds in the environment. The ear canal funnels the sounds to your eardrum.
- Middle ear: The sound from the ear canal hits and vibrates the eardrum – a membrane that divides the outer ear from the middle ear. The eardrum is connected to a series of three tiny bones. These bones are the malleus (“hammer”), incus (“anvil”), and stapes (“stirrup”). As the eardrum moves, so do the tiny bones.
- Inner ear: The third bone in the series of tiny bones in the middle ear is connected to another thin membrane that divides the middle ear from the inner ear. The inner ear consists of a spiral-shaped structure known as the cochlea (“snail shell”). Within the cochlea, there are thousands of tiny cells, known as hair cells. These hair cells are stimulated and send messages to the auditory nerve.
- Auditory nervous system: The auditory nerve runs from the cochlea to a station in the brainstem. From that station, neural impulses travel to the temporal lobe of the brain where the impulses are interpreted.
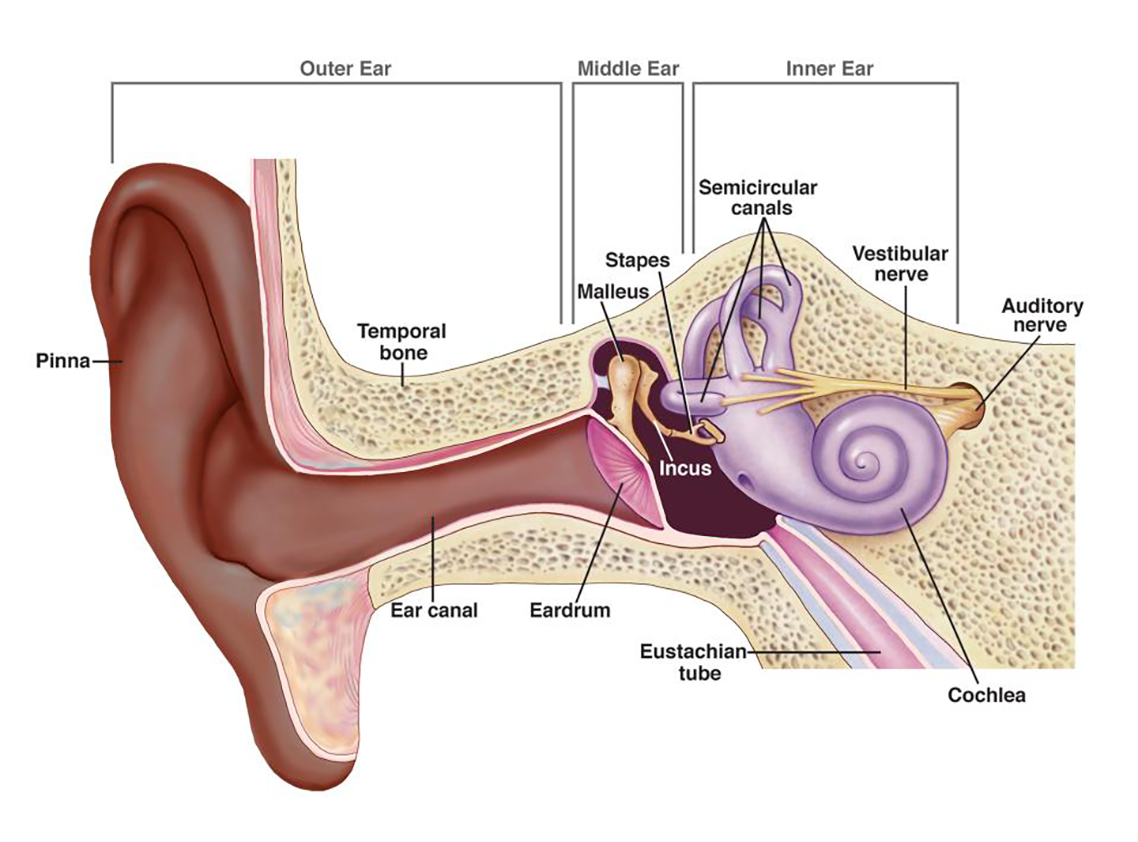
Image from: National Institute on Deafness and Other Communication Disorders, USA (2022) How do we hear?
What is ototoxicity, and what are ototoxicants?
Back to topOtotoxicity is “ear poisoning” caused by drugs or chemicals that target auditory or hearing functions. The agents that cause ototoxicity are called ototoxicants. They can affect or damage the auditory system – even when there are no loud noises - resulting in hearing loss and balance problems. Based on the part of the auditory system they damage, ototoxicants are grouped as follows:
- Cochleotoxicants mainly affect the cochlear hair cells, which are the sensory receptors, and can impair the ability to hear
- Vestibulotoxicants affect the hair cells on the spatial orientation and balance organs
- Neurotoxicants damage the nerve fibres that interfere with hearing and balance
How do ototoxicants damage the auditory system?
Back to topCurrently, ototoxicants are believed to affect or damage the auditory function by several different mechanisms, including:
- impairing the structure or function of the cochlea by:
- causing degeneration of the hair cells
- disrupting the membrane structure
- causing changes in the delicate vestibular hair cells
- disrupting the blood supply (ischemia) and reducing oxygen levels (hypoxia)
- simultaneously affecting the cochlea and the central auditory pathways
- affecting the auditory, optic, and vestibular nerve fibres of the central or peripheral nervous system (CNS)
What are possible health effects from ototoxicants and what are the symptoms?
Back to topThe main health effects are to hearing and balance even when the worker’s exposure is below the regulated occupational exposure limit for noise. Effects may be temporary or permanent.
It is important to note that in cases of exposure to noise and ototoxicants at the same time, noise levels may NOT need to be above exposure limits for the combined effects to be seen. In addition, impulse noise may be more harmful than continuous noise in the presence of some solvents.
Symptoms that may be related to hearing loss OR exposure to ototoxicants include:
- difficulty hearing in background noise
- hearing others’ speech as “mumbled”
- needing to ask others to repeat their conversation
- trouble hearing consonants
- speaking too loudly or too softly
- feeling like the volume needs to be louder to hear clearly
- tinnitus (ringing, chirping, buzzing, etc.)
- hyperacusis (heightened sound sensitivity)
- feelings of ear fullness
- oscillopsia (blurry vision with head movement)
- dizziness
- motion sickness
- unsteadiness when walking (especially in the dark or on dynamic surfaces like grass, gravel, uneven pavement, etc.)
- falls
- reduced mobility
Please see the OSH Answers “What makes chemicals poisonous?” for more information.
What chemicals cause ototoxicity?
Back to topMore than 100 substances present in workplaces have been identified as being potentially ototoxic. The structure or specific chemical properties needed to cause ototoxicity are NOT completely understood.
Substances that have been identified to be ototoxic or are strongly suspected to have ototoxic potential include:
- Organic solvents: Styrene, toluene, p-xylene, ethylbenzene, chlorobenzene, trichloroethylene, n-hexane, n-heptane, carbon disulphide, solvent mixtures
- Halogenated hydrocarbons: polychlorinated biphenyls, tetrabromobisphenol a, hexabromocyclododecane, hexachlorobenzene
- Nitriles: 3-Butenenitrile, cis-2-pentenenitrile, acrylonitrile, cis-crotononitrile, 3,3’-iminodipropionitrile
- Bromates: Sodium bromate, potassium bromate
- Metals and compounds: Lead, mercury, organotins, germanium dioxide
- Asphyxiants: Carbon monoxide, hydrogen cyanide, acrylonitrile, 3,3'-iminodipropionitrile
- Tobacco smoke
- Pharmaceuticals: Aminoglycosidic antibiotics (e.g., streptomycin) and some other antibiotics such as tetracyclines, loo diuretics (e.g., furosemide), certain analgesics and antipyretics (e.g., salicylates such as aspirin), certain antineoplastic agents such as cisplatin.
- Other substances: Pesticides (organophosphates, paraquat, pyrethroids, hexachlorobenzene), polychlorinated biphenyls, etc.
When ototoxicants can be absorbed through the skin (dermal), they are expected to have the following physicochemical properties:
- small molecules (molecular weight < 1000 g/mol (Daltons); some authors specify a molecular weight of <500 g/mol (Daltons)) that readily penetrate the skin), and
- Lipophilic (ability to combine with or dissolve in lipids or fats).
Examples of lipophilic substances with a molecular weight less than 500 g/mole (Daltons) are solvents such as hexane, benzene, toluene, styrene, chlorinated solvents (e.g., chloroform, tetrachloroethylene, carbon tetrachloride, methylene chloride), etc.
What is OTO notation and what is its purpose?
Back to topThe OTO notation is assigned to chemicals when they cause reversible or irreversible effects on the worker’s auditory system by one or more of the four main routes of exposure (e.g., inhalation, ingestion, skin absorption, or injection). The criteria for the OTO notation can vary for different jurisdictions and agencies. Generally, it is assigned when a chemical substance that can affect hearing or balance:
- On its own
- Due to combined exposure to a chemical and noise levels even below 85 dB
- Due to combined exposure to a chemical and noise that results in effects that are additive (the sum is what would be expected if exposed to each of the chemicals individually), potentiate (increases the likelihood), or synergistic (combined effect greater than the sum of the separate effects).
Chemicals are NOT assigned an OTO notation when:
- They cause neurotoxic effects without affecting hearing or balance
- There is a lack of or inconclusiveness of scientific evidence for ototoxicity
- The scientific evidence shows they are not ototoxic
The OTO notation is an alert for workplaces and users that the chemical or substance is ototoxic. The intention is for employers to focus attention on:
- exposure reduction
- placing affected workers in hearing conservation and medical surveillance programs to monitor their auditory capacity, even when exposures do not exceed the occupational exposure limits.
What workplaces use ototoxic chemical substances and which occupations may be exposed?
Back to topExposure to ototoxicants can occur in a wide variety of occupations as many ototoxicants are commonly used chemicals. Industries that use potential ototoxicants include manufacturing, mining, utilities, construction, and agriculture. Manufacturing and industries may include:
- Machinery
- Leather and allied product
- Textile and apparel
- Paper / Printing
- Chemicals (including paints)
- Plastics
- Furniture and related products
- Transportation equipment (e.g., ship and boat building)
- Electrical equipment, appliances, and components (e.g., batteries)
- Solar cell
- Manufacturing of metal, fibreglass, leather, and petroleum products
- Aircraft maintenance
- Assay laboratories
- Firefighting
- Pesticide spraying
- Fueling aircraft and motor vehicles
How does a workplace know if a hazardous product causes ototoxicity?
Back to topThe Workplace Hazardous Materials Information System (WHMIS) is a comprehensive system for providing health and safety information on hazardous products intended for use, handling, or storage in Canadian workplaces.
Ototoxicants can be identified by:
- Reviewing the Safety Data Sheet (SDS). If a hazardous product is ototoxic, it should be reported in the following sections of the SDS:
- Section 2 Hazard Identification
- Section 8 Exposure controls / Personal protection
- Section 11 Toxicological information
- Consulting the jurisdiction’s health and safety occupational exposure limits (OEL) list or the American Conference of Governmental Industrial Hygienists (ACGIH) Threshold Limit Values (TLVs® and Biological Exposure Indices (BEIs)® book under “TLV® Basis,”
- By researching the health hazards associated with ingredients in the product
NOTE: WHMIS does not have a specific health hazard class that corresponds directly to the OTO notation. The following WHMIS health hazard classes may be used by suppliers to report substances that are ototoxic or that have an OTO notation:
- Specific target organ toxicity – single exposure (STOT-SE) – Category 1 and 2 (special senses, hearing organs, all routes)
- Specific target organ toxicity – repeated exposure- Category 1 and 2 (special senses, hearing organs, all routes)
- Health Hazard Not Otherwise Classified (HHNOC) Category 1
What are the employer’s responsibilities for protecting workers from ototoxicants?
Back to topHealth and safety legislation in each jurisdiction requires employers to inform workers about known health hazards in their workplace.
Prepare a chemical inventory and record information about ototoxicity from:
- Supplier’s SDS (see Sections 2, 8 and 11) and technical literature. Ototoxicants may be listed as specific target organ toxicity, such as neurotoxicants, cochleotoxicants, or vestibulotoxicants
- Measure the amount of airborne ototoxicant to determine the workers’ exposure level
- Check your jurisdiction’s occupational exposure limits and whether it is assigned as an ototoxicant, either alone or in combination with noise. If the jurisdiction has adopted the ACGIH exposure limits, check the American Conference of Governmental Industrial Hygienists (ACGIH) current TLVs® and BEIs® booklet
- In absence of specific information from the manufacturer or if workers are reporting hearing or balance issues, search publicly available databases, government publications, and scientific databases for information on ototoxicity
Safe work practices include to:
- Carry out a hazard and risk assessment for products that are identified as ototoxicants and for those that are potential ototoxicants based on research data
- Document and investigate reports from workers about hearing loss. Explore whether ototoxicant exposure may be an issue and what can be done to reduce worker exposure
- Reduce the exposure to known or suspected ototoxic agents as a precautionary measure
- When there is a combined exposure to ototoxicants and noise:
- Reduce the 8-hour occupational exposure limit for noise to 80 dB (A-weighted). This recommendation is based on a precautionary principle
- Reduce the exposure level to the ototoxicants
- Require workers to wear hearing protection
- Based on good practices, ototoxic substances should be identified with a special label
- When exposure to ototoxicants occurs through dermal uptake, for which air concentration-based occupational exposure limits provide no protection, use biomonitoring for workers
- Prepare safe operating procedures and safe work practices based on the hazard and risk assessment and literature data
- Train the worker on the above procedures and practices and on the safe use and maintenance of personal protective equipment (PPE)
- Create an awareness program to educate workers about:
- ototoxicants used at the workplace
- ototoxicants outside of the workplace (e.g., medicines, and other non-occupational ototoxicants).
- the hazards of ototoxicants that also have a skin notation
- Establish a hearing conservation program, including audiometric hearing tests and monitoring. The program should be more thorough than what is traditionally carried out when only high noise levels are present. Recommendations include:
- Annual audiograms for workers whose airborne exposures, without regard to respiratory protection worn, are conducted when there is exposure to 50% of the occupational exposure limit, regardless of the noise exposure level
- Annual audiograms for workers where dermal exposure to an ototoxic substance is a concern
- Instructions for audiometric data reviewers. The reviewers should be alerted to:
- Possible additive, potentiating, or synergistic effects between exposure to noise and ototoxicants.
- Reports of hearing loss or other effects (such as loss of balance) when the audiometric test results are normal
- When comprehensive tests should be recommended to evaluate whether the more central parts of the worker’s auditory system are being affected.
- Implement control measures based on a hazard identification and risk assessment for a task and follow the hierarchy of controls:
- If possible, eliminate the use of ototoxicants
- If elimination of the ototoxicant is not possible, replace it with a less toxic chemical
- Implement engineering controls such as:
- Isolation and enclosures to control exposure to ototoxicants and noise
- Ventilation. Volatile ototoxicants should be used in chemical fume hoods or with other appropriate devices to ensure local capture of airborne ototoxicant.
- Implement administrative controls such as:
- Have a competent person prepare a hazard prevention program
- Audiometric testing to detect early signs of hearing loss, even in workers exposed below the action level for the ototoxicant
- Eliminate unnecessary tasks that cause noise or ototoxicant exposure
- Limit exposure time
- Schedule the operation of noisy equipment when workers are not nearby
- Personal Protective Equipment (PPE): Select the appropriate PPE according to health and safety legislation or industry safe practices. Use PPE such as head shields, goggles, glasses, gloves, coveralls, and boots. Remember that there is not a single type of material that is resistant to all products. Select the specific type of PPE to use based on the product present, the type of work completed, and the length of exposure. Get information from the manufacturer about how well their PPE performs against different products.
- Since many ototoxic substances can be absorbed through the skin, use chemical-protective gloves, arm sleeves, aprons, and other appropriate clothing
What are the worker’s responsibilities when working with ototoxicants?
Back to topWorker responsibilities include making sure they have received training and understand: How to look up the safe operating or safe work practices (if any) or SDS for the products they are using
- How to follow the instructions in the safe operating or safe work practices that relate to your tasks
- How to use, wear and maintain any required personal protective equipment (PPE)
- How to locate information related to WHMIS, emergency response, spill procedures, etc.
- Who to contact when the instructions are not clear or when unsure about any safe handling practices
- The personal hygiene practices that must be followed. Examples of personal hygiene practices are:
- Washing the skin regularly
- Wash contaminated clothing before wearing or wear clothing that is not soaked by chemicals or wear disposal coveralls
- Discarding contaminated clothing that cannot be washed
- Washing chemical-soaked clothing separately from your regular or other household clothing
- Not eating or drinking in work areas
- Cleaning and maintaining PPE according to the employer’s safe work practices or safety standards.
- When to report health and safety issues (such as hearing loss or balancing problems), or emergencies to your supervisor or employer.
- Fact sheet first published: 2023-02-06
- Fact sheet last revised: 2023-02-06

